Quality Podiatrist Care in Singapore
Leg & Foot Pain Clinic for Child & Adult
Trusted foot and lower-limb care experts — helping you walk, move, and live better.
A Member of Healthway Medical
Restoring Foot Health Through Podiatry
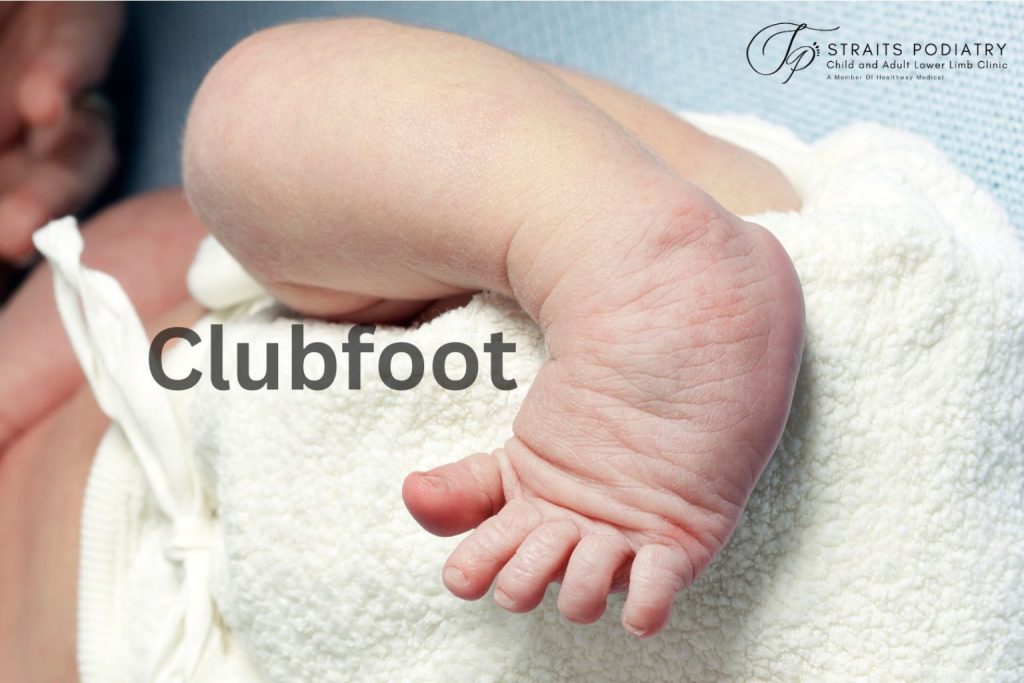
Straits Podiatry is the leading podiatry clinic in Singapore, providing dedicated care for patients of all ages. From paediatric concerns like flat feet and walking difficulties to adult issues such as lower limb musculoskeletal pain and soft tissue conditions, diabetic foot problems, and age-related mobility changes, our team offers personalised care across a wide range of podiatric conditions.
What is Podiatry?
In Singapore, podiatry is an allied health discipline that specialises in the diagnosis and management of most foot, ankle, and lower-limb conditions. Unlike foot and ankle surgeons, podiatrists offer a non-surgical approach when managing foot pain and walking abnormalities.
Foot & Leg Pain Conditions We Help With
NO STEROIDS, NO SURGERY, NO DOWNTIME
Our Philosophy in Lower Limb Care
At Straits Podiatry, we are focused on helping patients manage their conditions without the need for surgery. To tailor care to each individual’s needs, we first assess the underlying factors contributing to their condition. Tools like gait analysis help us identify biomechanical issues, while advanced technologies such as Extracorporeal Shockwave Therapy (ESWT) and Extracorporeal Magnetotransduction Therapy (EMTT) are applied to address concerns like muscular strain or joint discomfort to the leg or foot. By incorporating these non-invasive methods, we help patients improve their mobility, stay active, maintain independence, and return to sport.
Our Podiatrists
EXPERIENCED LOWER LIMB, FOOT AND ANKLE SPECIALISTS IN SINGAPORE
Mr Jackie Tey
Chief Podiatrist
Mr Jackie Tey started his Podiatry career at major hospitals in Singapore and spent years working alongside orthopaedic and vascular surgeons to manage complex foot conditions. His innovations and contributions in public hospitals have earned him international recognition and improved clinical outcomes for many patients. Mr Tey’s journey of becoming a podiatrist first began when he saw a Podiatrist for his flat feet and was intrigued by the profession.
Clinical Interest: Flat Feet, Foot & Knee Pain Conditions
Practice Location: Buona Vista
Qualifications:
- Bachelor of Podiatry (First Class Honours), Queensland University of Technology
- MOH Holding’s Health Science and Nursing Scholar, 2013
- Award Recipient for Orthotics and Clinical Studies by the Australian Podiatry Association
- Certified Medical Shockwave Practitioner by ISMST
- Certified Foot Mobilisation Practitioner
- Certified Dry Needling Practitioner of the Lower Limb
- President, Podiatry Association (Singapore) 2023/2024
Mr Benedict Khoo
Principal Podiatrist
Mr Benedict is a highly regarded Podiatrist in Singapore with many years of experience in private healthcare. Certified since 2017, he was one of the pioneers to use shockwave therapy and magnetotransduction therapy in Podiatry, harnessing innovation and technology to help his patients walk pain-free and return to sport. He was inspired to become a podiatrist while serving as a combat medic in the Navy, as he witnessed a large amount of lower limb injuries that military personnel went through.
Clinical Interest: Ingrown Toenail, Foot & Ankle Pain Conditions
Practice Location: Orchard
Qualifications:
- Bachelor of Podiatry (Second Class Honours), Queensland University of Technology
- Certified Medical Shockwave Practitioner By ISMST
- Certified Lower Limb Diagnostic Ultrasound Imaging
- Certified Sports Taping Practitioner
- Certified Ankle-foot Orthoses and Supramalleolar Orthoses Prescriber
Mr. Daniel Wong
Principal Podiatrist
Mr Daniel Wong has extensive experience managing complex foot and lower limb conditions across both public hospitals and private practice in Singapore. He is known for his precise clinical assessments and evidence-based treatment plans that focus on long-term outcomes rather than temporary relief.
His clinical approach integrates advanced biomechanics, rehabilitative principles and modern medical technology to deliver personalised, outcome-driven care. Patients frequently commend his warm, patient manner and his clear and professional explanations, which help them feel confident throughout their treatment journey.
Clinical Interest: Ingrown Toenails, Foot & Ankle Pain, Plantar Warts
Practice Location: Buona Vista & Katong
Qualifications:
- Master of Public Health, NUS
- Bachelor of Podiatry (First Class Honours), University of South Australia
- CEO Service Award, Singapore General Hospital
- SGH Overseas Merit Scholarship for Podiatry, 2012
- Chancellor’s Letter of Commendation, University of South Australia
- Certified Foot Mobilisation and Manipulation Therapy Practitioner level II
Our 4-step process to recovery
What To Expect On Your First Podiatry Visit
1. Understanding Your Condition
Our podiatrists will listen to your concerns and ask you necessary questions related to the condition. No rushed consultations, no guesswork.
2. Thorough Clinical Assessment
Our podiatrists will perform necessary clinical tests and thorough examination of your lower limb to diagnose your condition. This may involve using diagnostic ultrasound imaging.
3. Tailored Treatment Plan
Our podiatrists will provide a clear explanation of what's causing your symptoms and recommend the best care plan tailored to your lifestyle and needs.
4. Receive Your Treatment
We provide same-day diagnosis and treatment. Upon receiving your consent, our Podiatrist will start your treatment.

What Our Patients Say
Quality and dedicated foot care as shown in hundreds of reviews
Convenient Podiatry Clinics In Singapore
Multiple clinic locations
Easily accessible by MRT & public transport
-
31 Rochester Dr,
#02-01 (Hotel Block),
Singapore 138637 - CC22/EW21 Buona Vista
-
Monday to Saturday: 9 a.m. to 6 p.m.
Closed on Sunday & Public Holidays - (+65) 6990 4574
- hello@straitspodiatry.com
-
The Centrepoint
176 Orchard Rd,
#06-05,
Singapore 238843 - NS23 Somerset
-
Monday to Saturday: 9 a.m. to 6 p.m.
Closed on Wednesday, Sunday & Public Holidays - (+65) 6990 4574
- hello@straitspodiatry.com
-
i12 Katong, Core Collective
112 East Coast Rd,
#03-01/02/03/04/28,
Singapore 428802 - TE26 Marine Parade
-
Monday to Saturday: 9 a.m. to 6 p.m.
Closed on Wednesday, Sunday & Public Holidays - (+65) 6990 4574
- hello@straitspodiatry.com
Early care matters
Don't Neglect Your Feet..
Foot and lower limb pain often starts small — but when left untreated, it can affect your walking pattern, overall posture, knees and hips, and daily activities. Early podiatric care can keep you on your feet, stay active, and prevent more serious problems later.
Foot Health Blog
Latest updates from our podiatry clinic
Common questions
Frequently asked questions about our clinic
Do Your Podiatrists See Children?
Yes, and we also give talks to paediatricians to raise awareness of children’s foot health. Paediatric podiatry is essential for children, particularly those struggling to keep up with their peers in terms of development.
Children’s foot conditions are managed differently from those of adults because children are still growing. Therefore, your podiatrist must know how to identify and differentiate between a child’s normal and abnormal development to manage their problems effectively.
At Straits Podiatry, we understand that your child may feel nervous about attending our clinic. As such, we have a dedicated children’s assessment area designed to help your child feel at ease during consultation. Our podiatrists in Singapore are highly experienced in children’s foot conditions and can provide the best management advice for your child. We aim to educate and provide all parents with the right information so that their children do not undergo any unnecessary treatment.
Where are Straits Podiatry clinics located?
Our podiatry clinics in Singapore are located in the western region at Buona Vista, the eastern region at Katong, and the central region on Orchard Road. These locations serve patients across the West Coast, Central, and East Coast areas.
West Coast Region – Straits Podiatry (Buona Vista)
Address: 31 Rochester Drive, #02-01 (Hotel Block), Singapore 138637.
Nearest MRT station: Buona Vista (EWL/CCL) (Exit A or Exit D)
Notes:
- If you’re coming from the Park Avenue Rochester Hotel, take the lift lobby to level 2, exit via the meeting room, and turn left to reach the clinic.
- If you’re coming from Rochester Mall, take the link bridge at level 2 that connects to Park Avenue Rochester Hotel, and you’ll see our clinic on the right.
Central Region – Straits Podiatry (Orchard Road)
Address: 176 Orchard Rd, #06-05, Singapore 238843
Nearest MRT station: Somerset (NSL)
Notes:
- We are located within The Centrepoint shopping mall on level 6.
East Coast Region – Straits Podiatry (Katong)
Address: 112 East Coast Rd, #03-01/02/03/04/28, Singapore 428802
Nearest MRT station: Marine Parade (TEL)
Notes:
- We are located at Core Collective, i12 Katong level 3.
Do I need a referral letter to see a podiatrist in Singapore?
No, a medical referral letter is not required for a visit to a private podiatry clinic in Singapore. If you have a lower limb concern, you may contact us directly to schedule an appointment with us.
However, if you have a referral letter from a doctor regarding your foot issue, it is recommended that you bring it along to your appointment. This will generally help us better understand your foot condition. It might also help you seek reimbursement if your insurance provider requires one.
At Straits Podiatry, we receive referrals from medical doctors for various lower limb conditions. If your insurance policy states that a referral letter is needed before you can claim for podiatry treatments, you may consult any of Healthway Medical’s General Practitioners to obtain one before your visit.
What should I bring for my first podiatry consultation?
You may bring along all your past medical reports and medication list before a consultation with one of our podiatrists. These include any imaging scans (e.g x-ray or MRI) and their written reports. This will enable us to provide the best holistic care when addressing your concerns. You should bring along your frequently worn shoes, which include school shoes, work shoes, and regular sports shoes.
For parents seeking podiatry services for their children, please also bring their health booklet to the first visit. This will help us understand your child’s birth and developmental history.
Do you accept insurance or company medical benefits?
Coverage depends on your insurer and policy. Some policies allow patients to claim their consultation and treatment fees under outpatient or allied health benefits. Given the wide range of insurance policies available in Singapore, we are unfortunately unable to guarantee your coverage. We recommend checking directly with your insurer regarding coverage for podiatry services.
However, if you value high-quality care for your foot and lower limb concerns over the generosity of your coverage, you may contact us directly to book an appointment. Our fees are transparent, and all recommended care plans will be clearly explained to you before commencement. Our team will be happy to provide supporting documentation for you to try seeking reimbursement after.
How do I know if Straits Podiatry is the right clinic for me?
At Straits Podiatry, we value quality and comprehensive care. Our consultations focus on thorough assessment, clear explanation, and personalised care. We allocate sufficient time for proper evaluation rather than rushed visits.
So if you value a clear understanding of your condition and a well-explained personalised plan, rather than quick, generic consultations, Straits Podiatry will be a good fit for you.