What is Achilles Tendonitis?
You head out for a jog or climb a flight of stairs, and a dull ache starts to rise at the back of your ankle. Instead of fading, it lingers after activity, and even the simple act of standing on tiptoe can set it off again. It’s no coincidence that the phrase “Achilles heel” has come to mean a point of weakness, since this tendon, though built for strength, often becomes the body’s most fragile link. Because of this, the condition is commonly described as Achilles tendonitis or tendinitis, and in medical settings you might also hear the term tendinopathy, which is a blanket term for conditions affecting the tendon — tendinitis, tendinosis and tenosynovitis.
Since the tendon is engaged in every step, even routine movements can add to the strain. A sharp increase in running, long hours on unforgiving ground, stiff calf muscles, or shoes that lack proper support all place extra load on it. As these stresses repeat, the tendon fibres slowly lose their natural resilience, leaving the ankle in pain, especially after rest.
Because this process builds gradually, it’s best not to ignore persistent aches. A careful assessment can confirm whether the Achilles tendon is truly the source and rule out other causes. From there, a podiatrist can guide you with a plan that considers your activity levels, choice of footwear, and movement patterns, helping you manage the condition safely. With this context in place, it’s time to look closely at the symptoms of Achilles tendonitis.
Symptoms of Achilles Tendonitis
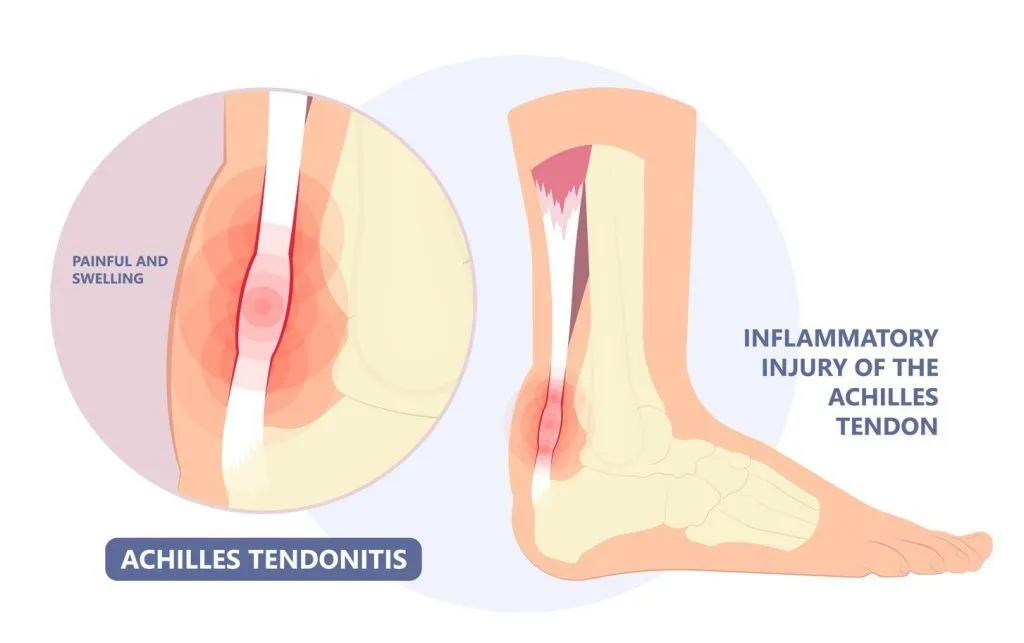
Symptoms of Achilles tendonitis often build up gradually, which is why the earliest changes can be easy to dismiss. What begins as a dull ache or pain at the back of the heel or ankle might become more persistent after exercise, and mornings can feel especially difficult when the tendon stiffens after inactivity. As the condition progresses, swelling, warmth, or even a small lump might appear, reducing flexibility and making everyday activities less comfortable.
Because the condition is not always presented in the same way, it’s important to understand that there are two main types.
- Non-insertional Achilles tendonitis – affecting the middle portion of the tendon, it leads to swelling and thickening. This is more common among younger, active people.
- Insertional Achilles tendonitis – this occurs where the tendon attaches to the heel bone, and this type can happen to any age group.
Note: In both types, repeated stress may also cause calcification, a process where damaged fibres harden and lose elasticity.
Recognising how these symptoms develop is important, since some patterns suggest the problem should not be ignored. Difficulty bending the ankle, struggling to walk comfortably, or swelling that spreads into the calf are warning signs of more significant strain. Pain that lingers for several days, disturbs rest, follows an injury with deformity, or is accompanied by redness, warmth, or fever are also signals that the problem should be reviewed without delay.
Causes of Achilles Tendonitis
Knowing what Achilles tendonitis feels like is only part of the picture. To understand how it develops, it helps to look at the stresses that can strain the tendon and the traits that raise the chances of it happening. While the condition might seem sudden, it is usually the result of repeated patterns that gradually wear down the tendon’s resilience over time.
Need Help? See A Podiatrist Today
What Strains the Achilles Tendon?
- A sudden rise in activity, such as longer runs, hill training, or high-impact sports with frequent jumping.
- Long hours on hard or uneven ground, especially without breaks.
- Shoes that are worn out or lack proper support for running or sport.
- Tight calf muscles with limited ankle motion, this places more strain onto the tendon.
- Reduced tendon elasticity with age, making it less resilient to repetitive stress.
- A direct injury or misstep that overloads the tendon suddenly.
Who Carries Higher Baseline Risk?
- Age between 30 and 50, though insertional tendonitis can occur at any age.
- Men are affected more frequently than women.
- Higher body weight, which places greater strain on the tendon.
- Athletes in sports with repetitive impact, such as running, football, or basketball.
- Foot mechanics such as flat feet (pes planus) or high arches (pes cavus).
- Bone spurs at the heel that rubs against and irritates the tendon.
- Health associations, including high blood pressure, diabetes, or psoriasis.
- Certain antibiotics (fluoroquinolones), which have been linked with tendon problems.
- Inadequate warm-up or stretching, particularly when calf muscles are tight.
Having outlined what contributes to Achilles tendonitis, the next step is to see how daily habits and care strategies can make a difference.

Managing and Preventing Achilles Tendonitis
Once the strains and risks are clear, the next step is to reduce the load on the tendon while building its capacity to cope with movement. Management begins with easing irritation, then progresses to restoring flexibility and strength so the tendon becomes more resilient. A podiatrist can tailor this approach around your activities, footwear, and routine, pacing recovery so that improvements feel steady rather than stop–start.
To begin, focus on measures that reduce irritation while supporting recovery:
- Activity changes that ease painful spikes yet keep you moving.
- A programme of gentle calf stretches and progressive strengthening for the calf and foot.
- In some cases, non-invasive therapies such as Extracorporeal Shockwave Therapy (ESWT) are used to stimulate the natural healing process in the tendon.
In parallel, make each step kinder to the tendon by improving how forces are managed:
- Supportive shoes with cushioning and good heel support to soften impact.
- Custom insoles (orthoses) or shoe modifications that distribute pressure more evenly and reduce excess strain.
- Avoiding worn-out shoes and ensuring regular warm-up and stretching, especially for the calves.
If symptoms persist despite consistent care, additional options may be considered:
- Adjunct therapies such as Platelet-Rich Plasma (PRP) or prolotherapy to encourage tendon healing.
- Surgery, which is uncommon and reserved for cases where the tendon does not improve with conservative measures.
Note: Corticosteroid injections are not advised, as they increase the risk of tendon rupture.
Finally, prevention helps to lock in recovery and lower the risk of setbacks. Start by increasing activity gradually, balancing higher-impact sessions with lower-impact options such as cycling or swimming. Alongside this, keep the tendon flexible and strong through regular calf stretches, strengthening exercises, and ankle mobility work. Supportive footwear and orthoses should also be maintained or replaced when worn, since they reduce daily strain. By combining these habits, the tendon becomes more resilient and less likely to flare up again

Have Your Achilles Tendonitis Managed at Straits Podiatry
Achilles tendonitis often starts as a mild tightness or occasional ache that gradually becomes more persistent. Over time, it can dictate your movements and limit the confidence you once had in your stride. Because this discomfort rarely comes from a single cause, it is important to understand the different factors that combine to strain the tendon over time. At Straits Podiatry, we begin with a thorough assessment that looks not only at the tendon itself but also at footwear support, calf flexibility, training load, and the surfaces you move on, so the underlying patterns are clear.
Once the factors are identified, we will work with you to design a care plan that fits into daily life. This might involve progressive calf loading exercises, pacing activities to avoid flare ups, and making footwear or insole adjustments to share the load more evenly. If symptoms remain persistent, non-invasive therapies such as ESWT can be considered as part of a broader care pathway. Book an appointment with us today and let’s take the first step toward easing pain and restoring your confidence in movement
Frequently Asked Questions on achilles tendonitis
What is Achilles tendonitis?
How many types of Achilles tendonitis are there?
What should I avoid doing when I have Achilles tendonitis?
If you have Achilles tendonitis, avoid activities that place excessive stress on the tendon such as running, jumping, or sudden increases in training. It’s also best to steer clear of worn-out or unsupportive footwear. Do not skip warm-ups or stretches, as these can worsen strain. For personalised guidance, seek advice from a podiatrist who can assess your condition and recommend safe strategies for recovery.