What is Plantar Fasciitis?
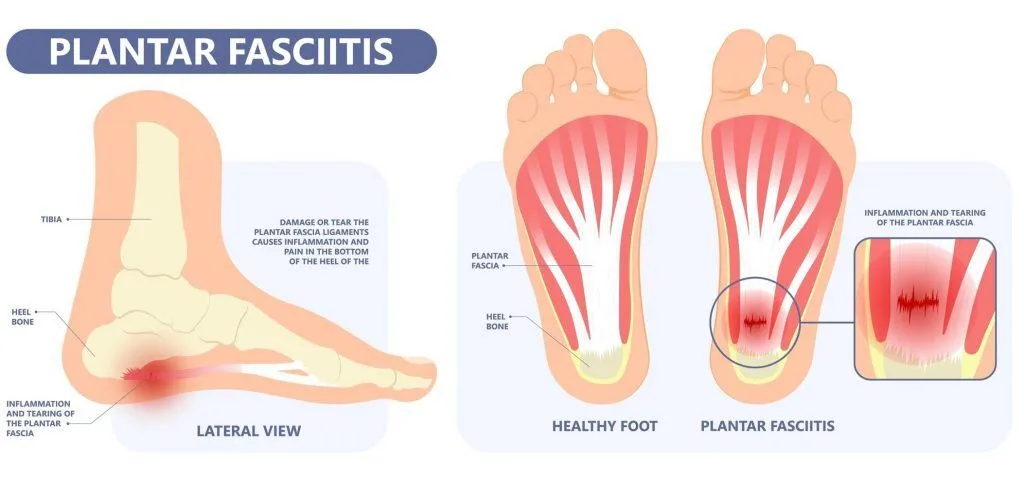
You swing your feet out of bed and a sharp jab under the heel stops you. In those first steps of the morning at home you feel it bite, and worry sets in as you wonder what kind of treatment to seek to alleviate the discomfort. Because heel pain has many causes, one possibility is irritation of the plantar fascia, the strong band that supports the arch.
To make sense of it, consider what loads this tissue. In particular, common heel pain causes include a sudden rise in activity, long hours on hard floors, tight calf muscles, and foot mechanics that strain the arch. As a result, when the plantar fascia is irritated, the first step after rest often feels especially sharp.
Given these patterns, it’s sensible to seek a clear assessment rather than guess. A podiatrist can review your foot mechanics, training load and footwear, then tailor a care plan that fits your goals and routine. But first, let us look at the symptoms of plantar fasciitis.
Symptoms of Plantar Fasciitis
To start, most people notice sharp, stabbing heel pain with the first few steps after waking. Similarly, the pain can flare up with the first steps after any spell of rest such as a long sit or car ride. As the foot warms, the pain often settles for a while, which can be misleading.
However, as the day goes on, discomfort commonly returns as a dull ache after longer walks or prolonged standing. The sore spot is usually on the underside of the heel, slightly toward the inner side, and pressing there often reproduces the pain.
Less commonly, there might be swelling around the heel that can extend toward the ankle, and in longer duration cases some people describe a burning or tingling sensation. Importantly, if there is a sudden snap or pop with severe pain and difficulty bearing weight, that can indicate a tear and needs prompt assessment.
Need Help? See A Podiatrist Today
Causes of Plantar Fasciitis
Having recognised that heel pain often bites with the first steps after any rest, it helps to understand why the tissue protests. The plantar fascia links the heel to the toes, supports the arch, and steadies each stride. When repeated tension and compression outpace recovery, microtears and local irritation build. After rest the plantar fascia and calf complex can be less supple, so the first reload places relatively greater stress on the heel.
What Increases Load on the Plantar Fascia?
- A new or rapid rise in activity, especially longer runs, jumping, or dance.
- Long hours of standing or walking on hard floors such as tile or marble. Colder floors or very cool rooms can tighten tissues, and barefoot steps can sharpen that first load.
- Shoes that are worn out or lack support.
- Reduced heel fat pad cushioning.
- Tight calf muscles with limited ankle motion.
- Leg length difference.
Who Carries Higher Baseline Risk?
- Age between 40 and 60.
- Higher body weight.
- Foot mechanics such as flat feet (Pes Planus) or high arches (Pes Cavus).
- Occupations that keep you on your feet for many hours.

Managing and Preventing Plantar Fasciitis
With the symptoms recognised and the causes understood, the guiding idea is clear. First, calm the irritated plantar fascia. Next, rebuild strength and flexibility so the same activities place less stress on the heel. A podiatrist will tailor this care plan to your pattern of pain, daily routine and goals, then pace the steps so progress feels steady rather than stop start.
To begin, focus on measures that settle pain while restoring capacity:
- Activity planning that smooths painful spikes yet keeps you moving.
- A rehabilitation programme with gentle plantar fascia and calf stretches, followed by progressive strengthening of the foot and calf.
- In selected cases, a night splint to lessen that first reload after rest.
In parallel, make each step kinder to the heel by improving how forces are managed:
- Supportive shoes with thicker soles and good cushioning to soften heel strike and reduce microtrauma throughout the day.
- Custom insoles (orthotics) that are designed to distribute pressure and, when appropriate, reduce excess pronation for more efficient mechanics.
If symptoms persist despite consistent care, targeted options can help where progress has stalled:
- Extracorporeal Shockwave Therapy (ESWT) aims to stimulate repair in stubborn cases.
- Steroid injections might offer brief respite, but it can weaken the fascia and raise tear risk.
- Surgery is uncommon and generally reserved for severe cases such as a complete tear or pain that does not settle after prolonged non-surgical care.
Finally, prevention consolidates the gains. Replace worn shoes and use supportive house footwear on hard floors. Increase training gradually and mix in lower impact sessions. Keep calves flexible and ankles mobile and practise simple foot strength work regularly. After any long periods of rest, ease into the first few steps to let tissues warm. Maintaining a healthy weight also reduces day-to-day strain. Taken together, these habits reduce load, build resilience, and lower the chance of a setback.

Have Your Plantar Fasciitis Pain Managed at Straits Podiatry
When heel pain starts to dictate your day’s activities, you don’t have to guess your way through it. At Straits Podiatry we first confirm the diagnosis, then connect the dots between your activities, choice of shoes, calf flexibility, foot mechanics, and the surfaces you tread on the most, so the reasons behind your pain are clear.
Frequently Asked Questions on plantar fasciitis
What is plantar fasciitis?
Who is at risk of heel pain from plantar fasciitis?
What are the types of plantar fasciitis?
What are the symptoms of plantar fasciitis?
Most feel a sharp pain under the heel. It is typically worst with the first few steps after waking or after any spell of rest such as a long sit, then eases as you move. As the day goes on, the discomfort often returns as a dull ache after longer walking or standing, and pressing on the tender spot near the front of the heel usually reproduces it. In longer standing cases there might be swelling or a burning or tingling sensation, but if you feel a sudden snap with severe pain and difficulty bearing weight, seek immediate assessment as this might be a tear.
Why see a podiatrist for plantar fasciitis heel pain?
Heel pain has many possible causes, so seeing a podiatrist helps you get the right diagnosis from the start. They specialise in the foot and can distinguish plantar fasciitis from conditions such as Achilles tendonitis, heel bursitis, or a stress fracture of the heel bone, which need different care. While a family doctor can assess you, pinpointing the exact source often requires a detailed review of foot mechanics, calf flexibility, footwear, and the surfaces you tread on regularly. A podiatrist then provides a clear care plan with footwear guidance, custom insoles, sensible activity pacing, and shockwave therapy if symptoms persist.



